
Getting Specific About Generic Drugs
It’s no surprise that generic drugs save you money.
844-655-0355 Our local experts have all your questions covered.
Questions about our plans? Call us at 844-655-0355, Monday – Friday 8 am to 6 pm.
Your ZIP code allows us to provide you with a personalized view of plans available in your area.
The ZIP code we have for you is 00000.
If this is not correct, fill out the form below for personalized plans available in your area.
Looks like the ZIP code you entered 66468 is outside the Blue KC service area.
Find coverage offered by Blue Cross and Blue Shield companies where you
live, or enter another Zip code below.
Please enter a valid ZIP code.
Please choose a county.
Call us Monday - Friday 8 a.m. – 6 p.m
844-655-0355
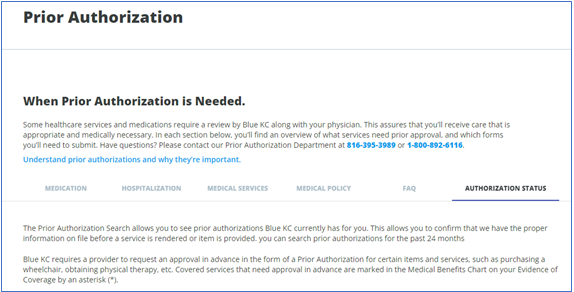
Blue KC wants you to receive the most effective, appropriate care and treatment available. We also want to protect you from incurring additional or unnecessary costs. That’s why we require your healthcare provider to get approval – also known as prior authorization – for certain services, medical procedures, and medications.
Your healthcare provider will submit a request for prior authorization via an electronic form, phone, or fax (contact information is on the back of your Blue KC member ID card).
NOTE: If you have pharmacy coverage through Blue KC, your physician must submit prior authorization requests for prescription drugs via electronic form.
Your physician’s office will submit:
Once the medical procedure has been approved, Blue KC will fax an authorization number, or a call the ordering physician or facility.
It’s the ordering physician or facility’s responsibility to complete the authorization process for your scheduled medical procedure. They can obtain verification by emailing prior_auth@bluekc.com.
IMPORTANT: Blue KC authorization does not guarantee claim payment. Services must be covered by your health plan, and you must be eligible at the time services are received. Claims submitted for unauthorized procedures are subject to denial.
Blue KC will notify the ordering physician or facility via fax and contact you in writing if the authorization is denied. We will provide a reason for the denial and information about how you can appeal the decision. This communication begins the appeal options per current state policy.
Blue KC also offers the ordering physician a consultation with a Blue KC medical director, known as the peer-to-peer process. The peer-to-peer process must be initiated within 24 hours of the denial notice and completed within seven days.
Following are some common questions regarding the Prior Authorization process:
Visit your member portal at MyBlueKC.com, click on Plan Benefits in the left column, then Prior Authorization for a complete list of procedures, products, services and medications that require prior authorization. You can also refer to your Medical Benefits Booklet in the Plan Benefits section of your member portal at MyBlueKC.com.
You can do your part by knowing what procedures, products, services, and medications require prior authorization, and confirming your provider has the correct information to submit on your behalf.
Log in to your member portal at MyBlueKC.com, click on Plan Benefits in the left column, then Prior Authorization. The Authorization status tab includes details on prior authorizations requested over the past 24 months:
Your coverage and plan payment are subject to your benefits and eligibility. Coinsurances, copayments, and deductibles may apply. Review your Medical Benefits Booklet at MyBlueKC.com, click on Plan Benefits in the left column, then Medical, or call Customer Service at the phone number on your Blue KC member ID card to verify your coverage.
Refer to your denial letter for next steps. Your provider may be able to conduct a peer-to-peer discussion. You, your provider or your designated representative may also be able to appeal.
All scheduled medical and surgical hospital admissions must receive prior authorizations.
If you have any questions, contact the Blue KC Prior Authorization team at 816-395-3989 or 1-800-892-6116. Or call the Blue KC Customer Service number on your member ID Card.

It’s no surprise that generic drugs save you money.

Drinking water prevents dehydration, which can cause unclear thinking, mood change, kidney stones, headaches, dizziness, heart palpitations, low blood pressure, overheating, or heatstroke.

Getting the right care at the right place and the right time is good for your health.